HEALTH HISTORY
A. BIOGRAPHIC DATA
NAME: Ms. CTS
ADDRESS: Binan, Laguna
AGE: 18 years old BIRTHDAY: 12 May 2000 BIRTHPLACE: Zamboanga City
SEX: Female RACE: Filipino/ Asian
MARITAL STATUS: Single RELIGION: Catholic
OCCUPATION: None
EDUCATIONAL LEVEL: College
CONTACT NUMBER: 09451369747
CONTACT PERSON: Mr. JS (Father)
CONTACT NO. OF CONTACT PERSON: 09209233688
DATE OF INTERVIEW: Dec. 15 2018
B. CHIEF COMPLAINT
Severe stomach pain and continuous vomiting approximately every 5 minutes that lasted for at least 1 hour
C. HISTORY OF PRESENT ILLNESS
Five months prior to consultation, the patient experienced stomach pain with the rate of 10 out of 10 after
drinking coffee from the Vendo machine while on her work immersion. When she got home, the pain progresses
and she eventually vomited at around 9 to 10 pm and lasted until around 1 am. She was then rushed to the clinic
in their subdivision due to hyperacidity and was diagnosed with gastric ulcers.
The night prior to consultation, the patient stated that she drank a caffeinated drink. The following
morning, around 10 a.m., she suddenly felt severe burning, sharp pain that caused her to wake up. She then drank
water and suddenly felt dizzy. The patient lied down for a while and used her phone and suddenly she felt the
need to vomit. She went to the comfort room and vomited. Her mother advised her to take medicine, which is
Maalox. So the patient drank the medicine with water yet still the patient vomited the ingested medicine. The
patient waited for a while in thought that the vomiting might stop. Then, her mother gave her Buscopan and the
patient drank it again with water. After that, the patient sat down and again felt the need to vomit. The patient
stated that she even tried to withhold her vomiting but still vomited. On the fourth time that the patient vomited,
she experienced burning sensations in her stomach. She was then brought to the clinic in her subdivision and
there, she was asked to undergo lab tests, specifically urinalysis, before they give her medicine. But due to
continuous vomiting, the patient wasn’t able to urinate. Her mother asked for her to be given dextrose because the
patient is starting to get dehydrated but the nurses in the clinic refused and said that the patient needs to be
admitted first but her mother personally wants to take care of the patient for they are a family of nurses. Later on
the nurses agreed to and put the patient on dextrose yet the patient still feels too dehydrated. The patient has been
given medicine too because she already urinated and the nurses also performed skin test (Buscopan). After that,
the patient is still not feeling well and still vomits. Night time came and the patient started to feel pain in her
stomach and then vomited again continuously. The following morning, she was brought to the clinic of a doctor
they personally know. She was asked to lie down and the doctor started palpating her stomach. The patient stated
that her whole stomach feels painful and sore when the doctor lightly palpated, but felt extreme pain when the
doctor deeply palpated her appendix area. She was then given antibiotics through IV. The following morning, the
pain subsided but still feels sore.
D. HISTORY OF PAST ILLNESS
PROBLEMS AT BIRTH: No known problems.
CHILDHOOD ILLNESSES AND ALLERGIES: Lactose intolerant (toddler years), German Measles (2010),
Frequent toncillitis (11 yrs old – 13 yrs old) Asthma (since birth), Hyperacidity with medications of Maalox
(2015)
IMMUNIZATIONS AT BIRTH: Complete
ACCIDENTS AND INJURIES: Foot sprain (2011 & 2015)
E. FAMILY HISTORY
Male, dead Female, alive client
Male, alive
Female, dead
FATHER’S SIDE MOTHER’S SIDE
No idea of the COD: severe hypertensive COD: no idea
COD decubitus ulcer &
diabetes
Glycoma
hypertensive
Severe asthma
COD: cancer
Patient stated that all of her father’s siblings are
hypertensive
asthma asthma dyslexia
REVIEW OF SYSTEMS
SYSTEMS PATIENT’S FINDINGS
GENERAL HEALTH Usual state of health “healthy”
Episodes of chills Usual weight: 54kg
Episodes of weakness or malaise Has recently lost 3kg
Fatigue Height: 5”5’ft
Experiences common
colds once approximately
every two months. (patient
can not recall cause of
colds)
Easily experiences fatigue
when performing
strenuous tasks.
INTEGUMENT (SKIN) Usual condition of skin Skin usually dry
Care habits Pale skin
Previously diagnose and treated Has chicken skin on upper
disease arm
Colour changes Skin temperature is warm
Dryness to touch after performing
Lesions strenuous activity.
Masses Perspires easily
Odours No lesions
Temperature changes No masses
Texture changes No odours
INTEGUMENT (HAIR) Usual state of hair Normal hair color is dark
Alopecia or hair loss brown
Excessive growth or change in Experiences hair loss
distribution Hair is evenly distributed
Texture changes Dyed hair seven times
Use of dyes No texture changes
INTEGUMENT (NAILS) Usual state of nails Pinkish nail bed
Changes in appearance Nail’s free edge is thin and
Texture changes easily breaks
HEAD AND FACE Usual state of health Experiences dizziness
Dizziness when skipping meals
History of trauma Experiences migraine
Injuries before menstrual period.
Pain No history of trauma
Syncope No head injury
Unusual or frequent headaches No syncope
EYES Usual state of eyes Near-sighted
Pattern of eye examinations Astigmatism
Visual acuity 50/75 eye vision
Cataracts No cataracts
Changes in visual fields or vision No excessive tearing
Excessive tearing No Glaucoma
Glaucoma No Infections
Infections No Pain
Pain No Pruritus
Pruritus No Redness
Redness No Unusual discharge or
Unusual discharge or sensations sensations
Visual disturbances No Visual disturbances
EARS Usual state of ears “feeling ko mahina” as
Care habits stated by the patient
Use of prosthetic devices Does not use prosthetic
Discharge devices
Hearing ability No discharge
Infections No infections
Presence of excessive environmental No presence of excessive
noise environmental noise
Otalgia (ear pain) No otalgia
Buzzing or ringing No buzzing/ringing
Vertigo No vertigo
NOSE AND SINUSES Usual state of nose and sinuses Colds once approximately
Olfactory ability every 2 months
Discharge No Discharge
Epistaxis No Epistaxis
Frequency of colds No Obstruction
Obstruction No Pain in infraorbital or
Pain in infraorbital or sinus areas sinus areas
Post nasal drip No Post nasal drip
Sinus infection No Sinus infection
Sneezing Sneezing due to excessive
dust
MOUTH AND THROAT Usual state Visits the dentist every
Pattern of dental care four months
Pattern of dental hygiene Brushes teeth twice a day
Use of prosthetic devices Flosses
Abscesses Doesn’t use prosthetic
Bleeding or swelling of gums devices
Change in taste No Abscesses
Dryness No Bleeding or swelling of
Excessive salivation gums
Hoarseness No Change in taste
Lesions No Dryness
Odours No Excessive salivation
Pain No Hoarseness
Sore throat No Lesions
Voice changes No Odours
No Pain
No Sore throat
No Voice changes
NECK AND NODES Usual state Stiffness
Masses No node enlargement
Node enlargement No pain and swelling
Pain No Tenderness
Swelling No masses
Tenderness
BREASTS Usual state Pain in the breast during
Self-examination pattern menstrual period
Dimpling No discharges
Discharge No Dimpling
Masses No Discharge
Pain No Masses
Tenderness No Pain
No Tenderness
RESPIRATORY AND Usual state asthma
CARDIOVASCULAR Past diagnosis of respiratory or wheezing when allergies
SYSTEMS cardiovascular system disease occur and during asthma
Date of last roentgenogram and ecg attacks
and results palpitations when dizzy
Cough usually normal blood
Cyanosis pressure unless some
Dyspnea alterations occur
Edema no edema
Hemoptysis no hemoptysis
High blood pressure no pain
Orthopnea no sputum
Pain
Palpitations
Sputum
Stridor
wheezing
GASTROINTESTINAL Usual state Hyperacidity
SYSTEM Previous roentgenogram and results Abdominal pain due to
Abdominal pain gastric ulcers
Appetite Nauseous and vomits
Bowel habits when hyperacidity occurs
Change in stool color Eats 2-4 meals a day
Constipation Regular bowel movement,
Diarrhea normal stool color
Dyschezia Experienced constipation
Dyspepsia Had diarrhea
Dysphagia No Dyschezia
Flatulence No Dyspepsia
Food idiosyncrasies No Dysphagia
Hematemesis No Flatulence
Hemorrhoids No Food idiosyncrasies
Hernia No Hematemesis
Indigestion No Hemorrhoids
Infections No Hernia
Jaundice
Nausea
Previously diagnosed problems
Pyrosis
Recent changes in habits
Rectal bleeding
Rectal discomfort
Thirst
Vomiting
URINARY Usual state Urinates 3-5 times a day
Past diagnosed problems Drinks water
Usual pattern of urination approximately 1-3 liters a
Change in stream day
Dysuria Had urinary tract infection
Enuresis Normal urine color and
Flank pain odor
Frequency No Change in stream
Hematuria No Dysuria
Hesitancy of stream No Enuresis
Incontinence No Flank pain
Nocturia No Hematuria
Oliguria No Hesitancy of stream
Polyuria No Incontinence
Pyuria No Nocturia
Retention No Oliguria
Stress incontinence No Polyuria
Suprapubic pain No Pyuria
Urgency No Stress incontinence
Urine color change No Suprapubic pain
Urine odor change
GENITAL (FEMALE) Usual state Uses feminine wash
Frequency of pap smear and results Had menstruation year
Care habits 2013
Diagnosed problems Menstruates approximately
Dyspareunia 5 to 7 days a month;
Lesions regular
Menstrual history No pap smear
Vaginal discharge No Dyspareunia
Obstetrical history No Lesions
Sexual history No Vaginal discharge
• Ability to perform and enjoy No Obstetrical history
satisfactory sexual
intercourse
• Age at onset
• Infertility
• Number of sexual partners
and numbers of sexual
partners with multiple
partners
• Problems with sexual
function or sexuality
• Satisfaction with sexual
activity
• Sexual activity
• Sexual preference
• Sexually transmitted diseases
• Sterility
• Use of contraceptives
MUSCULOSKELETAL Usual state Back pain when tired and
Past diagnosis of disease after waking up
Extremities Menstrual cramps
• Coldness Neck stiffness
• Deformities Feels weak when skipping
• Discoloration meals
• Edema Extremities
• Intermittent claudication • No Coldness
• Pain • No Deformities
• Thrombophlebitis • No Discoloration
Muscles • No Edema
• Cramping • No Intermittent
• Pain claudication
• Weakness • No Pain
Bones and joints • No
Thrombophlebitis
• Back pain Muscles
• Deformities • No Cramping
• Fractures
• Heat
• Limitations of movements
• Pain
• Redness
• Stiffness
• Swelling
CNS Usual state Feels anxious at times
Past diagnosis of disease There are behavioural
Anxiety changes at times
General behaviour change Easily forgets irrelevant
Loss of consciousness information
Mood change No seizures
Nervousness No hallucinations
Seizures
Speech
Cognitive ability
• Changes in memory
• Disorientation
• Hallucinations
Motor
• Ataxia
• Imbalance
• Paralysis
• Paresis
• Tic
• Tremor
• Spasm
Sensory
• Pain
• Paresthesia
ENDOCRINE History of physical growth and Growth spurt after
development menarche
Adult changes in size of head, hands, Has dry skin
or feet Hair evenly distributed
Diagnosis of diabetes or thyroid Experiences postural
disease hypotension
Dryness of skin or hair Experiences weakness
Exophthalmos when skipping meals and
Goiter when sleep deprived.
Hair distribution No Polydipsia
Hormone therapy No Polyphagia
Hypoglycaemia No Polyuria
Intolerance of heat or cold
Polydipsia
Polyphagia
Polyuria
Postural hypotension
Presence of secondary sex
characteristics
Weakness
HEMATOPOIETIC Past diagnosis of hematopoietic Blood type O
disease Easily bruises
Anemia No anemia
Bleeding tendencies
Blood transfusion
Blood type
Bruising
Exposure to radiation
Lymph adenopathy
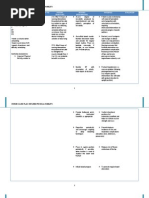
GORDON’S FUNCTIONAL PATTERN
BEFORE DURING
HEALTH PERCEPTION- • “Healthy naman ako, I get a • “I felt very weak.”
HEALTH cold every now and then • “Feeling ko na-limit ang
MANAGEMENT approximately every 2 months movement ko at sobrang
or something.” unhealthy ko.”
• “I usually just drink over the
counter medicines suggested by
my parents such as bioflu.”
NUTRITIONAL- • “May time na sobrang takaw ko • “I don’t feel like eating kasi
HEALTH and may time na sakto lang.” konti nalang kinakain ko pero
• “Nawawalan ako ng gana sinusuka ko pa rin kaya
kumain minsan.” dinextrose nila ako.”
• “Regular diet naman ako 2-4
rice meals per day, usually meat
and may times na hindi ako
nakakapagbreakfast”
• “Mahilig ako sa streetfood, like
inihaw”
• Pala-water din ako
approximately 1-3L per day
naiinom ko.”
ELIMINATION · “madalas every other day ako • “I didn’t have diarrhea naman
magpoop tapos color brown and di naman matigas yung stool
naman siya usually” ko, pero ang tagal nya lumabas.
· “Approximately mga 3-5 times Around 3 days.”
ako umiihi everyday.” • “dalawang beses lang ata ako
umihi sa buong 36 hours”
ACTIVITY- EXERCISE • “I can facilitate full-selfcare • “Ayoko tumayo at gumalaw for
naman.” about 3 days kasi ang sama nga
• “Di ako pala-exercise, yung ng pakiramdam ko.”
lakad lang pag nag-ttravel tsaka
pag papunta school.”
SLEEP- REST • “I sleep less than normal.” • “Halos 12 hours akong tulog,
• Falls asleep around 3-7am and nagising lang ako pag naiihi ako
wakes up around: 12 – 3pm or may nararamdaman.”
• “I read or watch documentaries • “Dahil sa ininom ko rin and yung
para makasleep pag nahihirapan binigay sa akin through IV so
ako matulog.” nagroggy na ako so nakakatulog
• “ soundtrip lang din ako pag ako dahil sa medicine”
walang ginagawa sabay
pahinga rin”
COGNITIVE- • “okay naman panrinig ko, wala • “ Maayos pa din naman pag-iisip
PERCEPTUAL akong glasses, malilimutin ako ko pero mas naoverwhelm kasi
when it comes to where ko ako sa sakit. Wala na nga akong
nilagay yung mga gamit ko .” masyadong matandaan aside sa
• “I have no difficulty in learning sakit.”
naman pero may times na
nababangag lang ako sa mga
nangyayare.”
SELF PERCEPTION- • “I think I’m just an average • “Nagsisisi ako na di ko inalagaan
SELF CONCEPT student.” yung sarili ko.”
• “I can be really emotional • “Ang weak ko ganun”
sometimes.” • “Hindi ko inexpect na at that
• “Sometimes I’m really point in my life, possible na
confident and then may times maoperahan na ako”
na mahiyain ako.”
• I’m aware na my body needs
exercise to be healthier.
ROLES- • “I have a lot of close friends rin • “Nung birthday ko naging
RELATIONSHIP and I don’t socialize with my worried sila. Tapos sila Francine
neighbors kasi di ako palalabas (her friend) sinama ako sa
around outside of our house at prayers nila”
puro matatanda kapit bahay ko • “since malaki ang family at
tapos kamaganak namin yung laging may away, di ako
katabi namin pero hindi kami masyadong nabibigyan ng
close kasi binackstab nila si attention nataranta lang sila kasi
mama.” parang isusuka ko na buong
• “I have a nuclear family where pagkatao ko”
my parents and 3 other siblings • “I made her worried pero still
fight a lot, kaya di kami stable naman yung relationship
masyadong close” namin”
• “I’m in a relationship with a
woman.”
SEXUAL- • “I had menstruation on year • “consistent pa rin naman since
REPRODUCTION 2012” kakamens ko lng noon
• “Last menstruation period was approximately 20 days ago, hindi
approximately 20 days ago, ako nagkaroon nung time na
mga 1 week tinagal” yon.”
• “Regular menstruation, 1 week
delay at most”
COPING- STRESS • “There are times na I drink • “I prayed to God while I was in
TOLERANCE alcohol to relieve stress .” the hospital.”
• “My gf and my older sister • “I sleep it off.”
helps me relieve the stress and • “Si Achi (her sister), siya talaga
they’re always there when I yung nagobserve sa akin, tapos
need them.” yung girlfriend ko emotional
• “My fears (bullying) affect me support”
too much and I think that it’s a • “napaka-fragile ko nun pero
big problem na.” nagging optimistic ako na hindi
• “I handle my problems by ako ooperahan, kakayanin to ng
either ignoring them or talking gamot”
it out, and being more
optimistic in life. They are
effective most of the time.”
VALUES- BELIEF • “I’m a roman catholic but I • “I prayed more than usual.
don’t usually go to church and Hoping na hindi matuloy yung
hindi rin pala-simba talaga ooperahan ako. Its either
family ko so hindi rin ako pampalakas ng loob ko yung
nasanay.” pagpray or I was hoping din
• “ayoko ding pumunta ng church talaga through faith.”
kasi nahihilo ako for some
unkown reason”
• “Hindi man ako palasimba pero
nagdadasal naman ako
everytime na umaalis ako tsaka
pag may mga challenges din
ako sa life tulad ng mga test at
struggles ko sa buhay.